 |
| Spinal Stenosis Explained - Quick Links: |
|
|
What is spinal stenosis?
Spinal stenosis is a narrowing of the spinal canal. Some patients are born with this narrowing, but most often spinal stenosis is the result of a degenerative condition that develops in people over the age of 50. Younger people with a spine injury or a narrow spinal canal are also at risk. Spinal stenosis is the gradual result of aging and "wear and tear" on the spine from everyday activities. Degenerative or age-related changes in our bodies can lead to compression of nerves (pressure on the nerves that may cause pain and/or damage). This crowding of nerve fibers results in pain and numbness in the back and legs when standing or walking.
What causes spinal stenosis?
Your spine, or backbone, protects your spinal cord and allows you to stand and bend. Spinal stenosis causes narrowing in your spine. The narrowing can occur at the center of your spine, in the canals branching off your spine and/or between the vertebrae, the bones of the spine. The narrowing puts pressure on your nerves and spinal cord and can cause pain.
Spinal stenosis is the gradual result of aging and “wear and tear” on the spine from everyday activities. Degenerative or age-related changes in our bodies can lead to compression of nerves (pressure on the nerves that may cause pain and/or damage).
As we age:
- the ligaments of the spine can thicken and calcify (harden from deposits of calcium)
- bones and joints may also enlarge
- bone spurs, called osteophytes, may form
- discs may collapse and bulge (or herniate)
- one vertebra may slip over another (called spondylolisthesis)
|
|
(mouse over the picture above to freeze the image transition) |
 Back
to top Back
to top
What are the symptoms of spinal stenosis?
If you suffer from lumbar spinal stenosis you may feel various symptoms, including:
- dull or aching back pain spreading to your legs
- numbness and “pins and needles” in your legs, calves or buttocks
- weakness, or a loss of balance, and
- a decreased endurance for physical activities
Symptoms increase after walking a certain distance or standing for a time. Symptoms can improve when you:
- sit
- bend or lean forward (see Figure below)
- lie down, or
- put your foot on a raised rest
 Back
to top Back
to top
How would I know if I had spinal stenosis?
Diagnosing Lumbar Spinal Stenosis
Before confirming a diagnosis of stenosis, it is important for your doctor to rule out other conditions that may produce similar symptoms. In order to do this, most doctors use a combination of techniques, including:
- History - Your doctor will begin by asking you to describe any symptoms you have and how the symptoms have changed over time. Your doctor will also need to know how you have been treating these symptoms, including medications you have tried.
- Physical Examination - Your doctor will then examine you and check for any limitations of movement in your spine, problems with balance, and signs of pain. Your doctor will also look for any loss of reflexes, muscle weakness, sensory loss, or abnormal reflexes.
- Tests - After examining you, your doctor may use a variety of tests to confirm the diagnosis. Examples of these tests include:
- X-ray - shows the structure of the vertebrae and the outlines of joints.
- MRI (Magnetic Resonance Imaging) - provides a three-dimensional view of our back and can show the spinal cord, nerve roots, and surrounding spaces, as well as signs of degeneration, tumors or infection.
- CAT Scan (Computerized Axial Tomography) - depicts the three-dimensional shape and size of your spinal canal and bony structures surrounding it.
- Myelogram - highlights the spinal cord and nerves after a dye is injected into your spinal column, which appears white on an X-ray film
Precaution: Radiological evidence of stenosis must be correlated with your symptoms before the diagnosis can be confirmed.
 Back
to top Back
to top
What are the treatment options for spinal stenosis?
Treatment Options
Once a diagnosis of spinal stenosis is confirmed, the process of treating the condition usually begins with a regimen of non-invasive, “conservative” therapy.
Non-surgical Treatment of spinal stenosis
There are a number of ways a doctor can treat stenosis without surgery, including:
- Medications, such as non-steroidal anti-inflammatory drugs (NSAIDs) to reduce swelling and pain, and analgesics to relieve pain.
- Corticosteroid injections (epidural steroids) to reduce swelling and treat acute pain that radiates to the hips or down the leg. Pain relief from an epidural injection may be temporary and patients are usually advised to get no more than 3 injections per 6-month period.
- Rest or restricted activity.
- Physical therapy and/or exercises to help stabilize the spine, build endurance and increase flexibility.
While some patients obtain relief from symptoms with these treatments, others do not.
Surgical Treatment of spinal stenosis: Decompression
Non-surgical treatments may temporarily relieve pain. More severe cases of stenosis may require surgery.
The most common surgical procedure for stenosis is a decompressive laminectomy sometimes accompanied by fusion. Often referred to as “unroofing” the spine, this procedure involves the removal of various parts of the vertebrae, including:
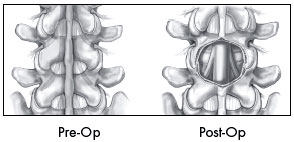 the lamina, as well as the attached ligaments, that cause compression of the spinal cord and nerve roots, and/or the lamina, as well as the attached ligaments, that cause compression of the spinal cord and nerve roots, and/or- enlarged facets, osteophytes and bulging disc material
The goal of the surgery is to relieve pressure on the spinal cord and nerves by increasing the area of the spinal canal and neural foramen.
Other types of surgery to treat stenosis include:
- Laminotomy - only a small portion of the lamina is removed to relieve local pressure on the spinal cord and nerve roots.
- Foraminotomy - the foramen (the opening through which the nerve roots exit the spinal canal) is enlarged to increase space for the nerves. This surgery can be done alone or with a laminotomy.
- Facetectomy - part of the facet joint is removed to increase space for the nerves
- Interspinous Process Decompression (IPD) IPD is a surgical procedure in which an implant, called the X-STOP®, is placed between two bones called spinous processes in the back of your spine. It is designed to remain safely and permanently in place without attaching to the bone or ligaments in your back.
back to top
|
|
 |
|